Abstract
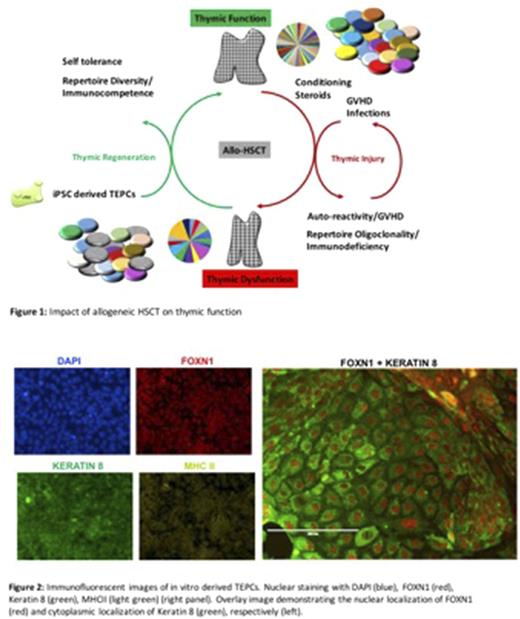
Hematopoietic stem cell transplantation (HSCT) remains the only curative therapy for many malignant and non-malignant diseases to date. The thymus plays a key role in post-transplant immune reconstitution. The outcome of a HSCT and the recipient thymic function are intimately intertwined. In fact, the production of mature T cells occurs in the thymus and depends on the interaction of hematopoietic progenitor cells with non-hematopoietic stromal elements, notably thymic epithelial cells (TECs). Through positive and negative selection, a healthy thymus generates a broad and self-tolerant T cell receptor (TCR) repertoire that protects from infection and prevents autoimmunity. In addition, the thymus gives rise to regulatory T-cells which confine immune responses and further promote central tolerance. At odds with its importance for successful transplant outcomes, the thymus is exquisitely sensitive to a wide range of insults encountered during the peri-transplant period, including cytotoxic agents, steroids and irradiation. In the allogeneic transplant setting, acute graft-versus-host disease (GVHD) can cause further thymic injury. Thymic injury in turn, leads to susceptibility to infections and autoimmune complications. Moreover, it is now widely recognized that thymic injury leading to defective deletion of self-reactive T-cells along with misguided T-helper cell polarization and B-cell activation constitute major drivers of chronic GVHD. Together these represent the leading causes of non-relapse-related transplant mortality and morbidity. As such, HSCT can precipitate a vicious cycle, in which the success of the HSCT procedure hinges on intact thymic function, but the HSCT process itself often causes irrecoverable thymic injury (Figure1). Thymic function naturally declines with age with little to no endogenous potential to regenerate. Current treatment options for thymic injury during HSCT are limited to symptomatic therapy. Therefore, novel approaches to cure irreversible thymic injury are critically needed.
To address this need, our goal is to generate fully functional thymic epithelial progenitor cells (TEPCs) from hPSCs as a stem cell-based therapy for thymic regeneration and restoration of immune competence in HSCT recipients. Building on the efficient induction of definitive endoderm from human pluripotent stem cells (hPSCs) by directing signals controlling lineage bifurcations, we have developed a novel platform that drives TEPC development through sequential induction of the intermediaries anterior foregut (AFG) and pharyngeal pouch endoderm (PPE). Here we show that TEPCs derived in vitro from hPSCs or hESCs express the key thymic transcription factor FOXN1 along with Keratin 5 and Keratin 8, the primary cytoskeletal building blocks of medullary and cortical TECs, respectively. In addition, in vitro derived TEPCs express MHC class II to varying degrees (Figure 2). To optimize our in vitro platform, modifications of key-signaling pathways in the differentiation protocol are validated by comparing the transcriptome of hPSC-derived TEPCs to that of primary human medullary and cortical thymic epithelial cells using next generation sequencing. Our ongoing work is testing the capacity of hPSC-derived TEPCs to promote T-cell maturation, positive and negative selection resulting in the development of a broad and self-tolerant TCR repertoire from adoptively transferred human HSPCs in a humanized mouse model.
Through sequential validation of fidelity, functionality, transplantability and sustainability of hPSC-derived TEPCs, we strive to develop an experimental model that can be translated by a clinical Good Manufacturing Practice (cGMP) facility for use in bone marrow transplant recipients.
Ultimately, the potential applications of in vitro derived TEPCs are not confined to restoring thymic function in the HSCT setting. TEPCs derived from solid organ donors hold the promise of inducing tolerance to donor tissues, thereby preventing rejection of the transplanted donor organ. Leveraging the body's own ability to educate T-cells through regenerating thymic tissues could represent a novel approach to addressing key challenges in transplantation immunology.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal